Michael D. Shear, from The New York Times, wrote an article published on December 28th titled Trump Weighs Letting Veterans Opt Out of V.A. Medical Care. Essentially, the article seizes on the meeting Trump had with healthcare experts about reshaping the VA hospital and its care. President-elect Donald J. Trump announced this week that he is considering a plan to allow military veterans to opt out of medical care at Veterans Affairs hospitals and instead see private doctors of their choosing.
Shear wrote, “Mr. Trump met on Wednesday afternoon with John H. Noseworthy, the president of the Mayo Clinic; Paul Rothman, the chief executive of Johns Hopkins Medicine; David Torchiana, the chief executive of Partners HealthCare; Delos Cosgrove, the chief executive of the Cleveland Clinic; and several others. The transition official said Mr. Trump was considering asking members of that group to form an advisory committee to help him reshape the V.A.”
The complexity of the conversation appears to be spawned by the elimination of essential Veteran Population Health data, lack of prioritization, and misunderstanding of the Veteran healthcare marketplace. The commercial hospitals essentially have three issues with the acceptance of VA Hospital patients: fee reimbursement, healthcare record sharing and data integration, and cultural competency and military-environment/clinical training. While there are hundreds of organizations focused on reimbursement and healthcare record management, there is only one organization, Maryland-based Warrior Centric Health (WCH), providing dynamically integrated solutions and tools that understand the importance of military and veteran culture, cultural competency, and effectively communicating with generations of service members, Veterans and family members in a clinical setting.
WCH has an accredited veteran-focused eLearning program in which expands a healthcare practitioner’s Veteran care. The WCH Hospital Recognition Program directly responds to Veteran Population Health goals and objectives. Together, both programs increase patient satisfaction ratings by improving care effectiveness, increasing operational efficiency, adopting data driven decision support and continuous improvement techniques, and deploying community outreach programs.
Warrior Centric Health CEO, Ron Steptoe, knows the public-private option being discussed is not only feasible but currently in place for over 70% of Veterans. The issue is not opting in Veterans as patients – the commercial hospitals already do accept Veterans. They just don’t know it. There are over 22 million Veterans in the United States with over 2.5 million deployed since 2001. In the last year, over 1.2 million service members left the military and returned to their homes in every corner of the country. Only 27% of Veterans receive some health care from the VA annually. Where do the rest go? Our local hospitals and medical practices.
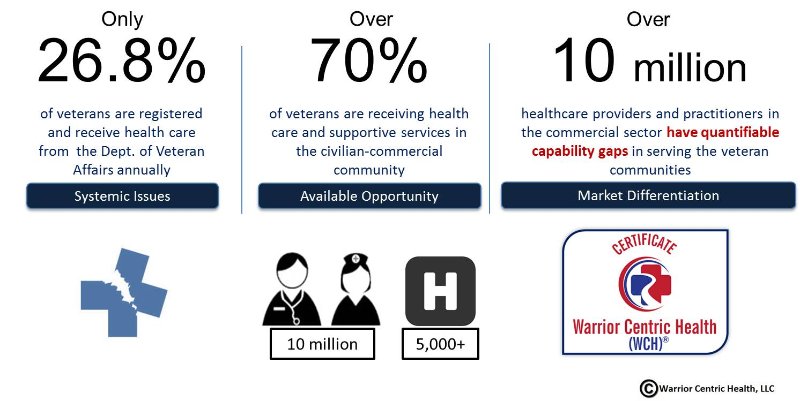
Veterans and their families – 74M strong – walk amongst us unnoticed. They are our neighbors living and working in every community and yet struggle for proper healthcare. Because of their unique needs, they often get undiagnosed, under-diagnosed and misdiagnosed in local hospitals which are unaware, untrained, and unable to properly and efficiently care for our Veterans. Veterans and family members represent about 25 percent of the U.S. population and signify an ongoing urgent need for healthcare providers and allied health team members to understand the specific challenges presented by those who have fought and sacrificed in our nation’s conflicts.
With Warrior Centric Healthcare Training, medical practitioners master unique clinical situations by exploring the differences in military service, military culture, rank, veterans, gender issues, age, values and beliefs, socio-economics, race, ethnicity and religion. Healthcare professionals requiring CME/CE credits as well as interested in obtaining foundational Veteran Population Health training for healthcare facilities and clinical practice as well as advanced clinical expertise and skills in Veteran health have access to accredited eLearning modules by the following medical learning organizations and Professional Associations:
- American Medical Association (AMA)
- American Association of Nurse Practitioners (AANP)
- American Nurses Credentialing Center (ANCC)
- American Academy of Physician Assistants (AAPA)
- Accreditation Council for Pharmacy (ACPE)
- Advancing Knowledge in Healthcare (AKH, Inc)
“We are proud to provide the critical knowledge, training, and tools needed to operationalize the commitment made by hospitals, systems, employer clinics, and medical schools to educate current and future medical professionals on the challenges and special needs of our military, veterans and their families,” said Steptoe, also a U.S. Army veteran.
Dr. Evelyn Lewis, MD, MA, FAAFP, DABDA, Chief Medical Officer of Warrior Centric Health and a U.S. Navy veteran commented that, “the Warrior Centric Health program is specifically designed to inform as well as enhance the knowledge, understanding, and skills of healthcare professionals on the culture, nuances and needs of the care provided for those who have served our nation.”
During a public appearance in 2015, Mr. Cosgrove, Cleveland Clinic, said that only private industry can solve runaway health care costs. He said that had to start with employers investing in the health of their workers. He also said, “We are not going to begin to control the cost of health care until we deal with things that cause chronic disease. The government is not going to do it.”
Warrior Centric Health (WCH) agrees and knows the answer to Veteran Population Health is to start with clinical staff in hospitals and practices investing in knowledge. WCH’s motto is “You Must Know Me To Treat Me” and that is the true bottom line in Veteran Health in the commercial sector.
Warrior Centric Health, LLC—named by Forbes as one of the Top 25 Veteran-Founded Start-ups in America—is the first accredited eLearning program to address the socio-cultural determinants of health in veterans and their families. Its design equips commercial and non-profit hospitals, medical personnel and staff with the skills necessary for the standard and consistent application of culturally competent methodologies when treating veterans and their families. WCH provides quality education, data science, credentialing, community outreach and market relationship support to improve long-term health outcomes for vulnerable populations.
For more information about Warrior Centric Healthcare Training: Warrior Centric Health, LLC and Warrior Centric Healthcare Training (WCHT).

